Prof. Findl has many years of experience in vitreo-retinal surgery. After several years of surgical experience at the Vienna General Hospital (AKH) he underwent intensive training in vitreo retinal surgery in the form of a fellowship in vitreo retinal surgery at Moorfields Eye Hospital in London. His additional training at this highly recognised institution has contributed to safety and experience in all fields of vitreo retinal surgery. With 150 – 200 vitreo retinal surgeries per year, Prof. Findl is one of the most experienced vitreo-retinal surgeeons.
Eye Surgery
Retinal Surgery
Vitreo-retinal Surgery
Diseases
Epiretinal Membrane
(Macular Pucker)
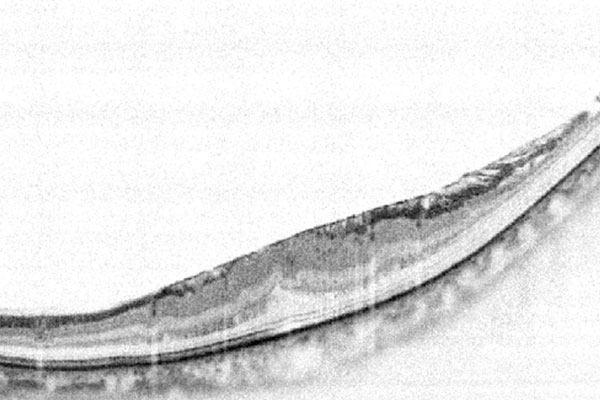
An epiretinal membrane, also called “Macular Pucker” oder “Cellophane Maculopathy”, is a thin membrane that overlies the centre of the retina, called the macula. This fibrous tissue grows on top of the inside of the central retina. Thereafter, it may contract and cause wrinkles and folds. Patients ususally notice their vision to deteriorate and may see straght lines slightly curved (metamorphopsia). This thin membrane may be visualized using a special examination technique called OCT.
What causes an epiretinal membrane?
In most cases, there is no obvious reason for the epiratinal membrane. In some cases, an epiretinal membrane may follow another eye disease. Examples are a previous retinal detachment, chronic inflammatory diseases such as uveitis, retinal tears and vascular occlusions.
How is an epiretinal membrane treated?
Should the epiretinal membrane result in compromised visual acuity or distorted vision, surgery is usually recommended. It is important to note that an epiretinal membrane is not the same as age related macular degeneration. Both deseases affect the centre of the retina, the macula, however are completely different entiyties and require different treatments. Since the epiretinal membrane can be operated, it has a better prognosis than macular degeneration.
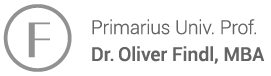
What happens during the peeling of the membrane?
Vitrectomy involves the removal of the vitreous body, a tranparent gel in the back of the eye which is usually liquified and plays no important role in the adult eye. Prof. Findl typically performs this surgery in local anaesthesia, nevertheless it can also be performed under general anaesthesia if the patient wishes. After removal of the gel, the epiretinal membrane is peeled using a fine forceps. Thereafter, the underlying very thin inner limiting membrane called ILM is stained with blue dye and also peeled off. Studies have shown that removal of the ILM results in better outcomes than only removal of solely removal of the epiretinal membrane. In many cases, air or gas are injected into the eye at the end of surgery. This gas bubble dissolves within a few days to weeks after surgery and is replaced by the physiological fluid produced inside the eye. In vielen Fällen wird noch Luft oder Gas als Tamponade ins Auge injiziert, welches sich dann in einigen Tagen bis Wochen von selbst auflöst und durch die eigene innere The 3 small iscisions of approximately 1mm in size are ususally self sealing, but in some cases may be secured with resolvable sutures.
What is the prognosis?
Within several days after surgery vision usually improves. It may take 3-6 months until the final visual acuity is reached. Concerning the prognosis of this kind of surgery, the main goal is to preserve the visual acuity and reduce visual distortions. In many cases, visual acuity can return to nearly normal, however perfect visual acuity is reached in only few cases. A side effect of vitrectomy is the development of a clouding of the lens, called cataract. This usually develops within several months up to few years after surgery. Cataract can be treated effectively with cataract surgery.
Macular Hole
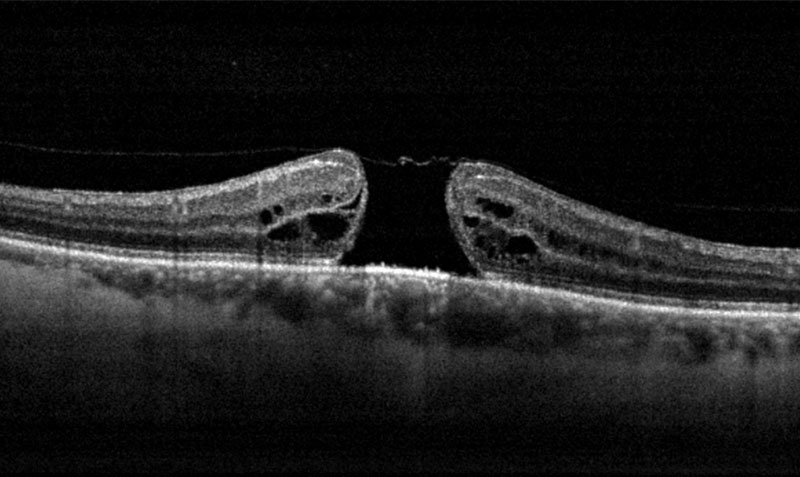
A macular hole, a hole in the centre of the retina, usually develops spontaneaously. A macular hole is diagnosed during the retinal examination at the slitlamp as well as the OCT.
What are the causes of a macular hole?
A macular hole, a hole in the centre of the retina, usually develops spontaneaously. This is often associated with a age related collapse of the vitreous body, the transarent gel in the back of the eye.A macular hole is diagnosed during the retinal examination at the slitlamp as well as the OCT. Shoud the macular hole affect visual acuity, surgery is recommended.
What happens during surgery?
During surgery, the first step is to remove the vitrous body of the eye. Prof. Findl typically performs this surgery in local anaesthesia, it may also be perfromed under general anaesthesia should the patients wish. Through three small openings, the vitreous gel is cut and removed. Thereafter, the very thin innermost layer of the retina, the inner limiting membrane, ILM, is stayned with blue dye and then removed using a fine forceps. Studies have shown that removal of the ILM may lead to better visual results after surgery. Lastly, a gas bubble is injected into the eye at the end of surgery to mechanically close the whole.
Which precautions do I have to take after surgery?
Following surgery, the patient shoud stay in a face-down position for 1 – 2 days. This helps to press the rim of the hole against the underlying layer and helps closure of the hole. Depending on the gas mixture used, the gas bubble will stay in the eye for 2 – 6 weeks, progressively diminishing in size. As long as the gas bubble is in the eye, vision is poor and the patient should not undertake airline flights.
What is the visual prognosis after surgery?
Thereafter, visual acuity may increase or at least stabilize. In many cases, it may take several months to reach the final visual acuity. Concerning the visual prognosis, the primary goal of this surgery is stabilization of visual acuity and improvement of visual distortions. The prognosis is dependent on the size of the macular hole before surgery. In the case of a large macular hole, visual prognosis is guarded. A side effect of vitrectomy is the clouding of the lens, also called cataract. Cataract ususally develops within several months to a few years after surgery. Cataracts can be treated effectively with cataract surgery.

Retinal Detachment (Ablatio retinae)
Typical symptoms of a beginning detachment are a sudden onset of numerous floaters (grey of black floating dots), flashes of light and the appearance of a grey or black “curtain” impeding the visual field. If you experience any of these symptoms, you should be seen by an ophthalmologist on the same day. If a break is detected early and the retina is still attached, laser treatment may suffice. Once the retina is detached, surgical treatment is needed.
What are the causes of retinal detachment?
Retinal detachment is usually caused by a retinal break, either a tear or a hoe. These typically develop after the collapse of the virteous body, a transparent gel at the back of the eye. This results in fluid flowing through the break under the retina and detaching it. Retinal breaks are more commonly found in myopic patients (shortsighted patients). Since the retina is in nead of nutrients and oxygen from the underlying layer, the retinal cells are severly damaged during a retinal detachment. Therefore, a retinal detachment should be treated urgently.
What happens during vitrectomy?
Nowadays, we most commonly use as the surgery of choice for retinal detachments. The vitreous body, that has caused the retinal break, is removed. This type of surgery is usually perfomed under local anaesthesia but may also be performed using general anaesthesia if the patient wishes.
During surgery, the vitreous body is removed through 3 small openings. Then, the retinal break is treated either with laser or local freezing (cryopexy) resulting in local scarring. which seals the break. Thereafter, a gas bubble or in some cases silicone oil is injected into the eye at the end of surgery, depending on the size and localisation of the break. After surgery, the patient needs to stay in a special position, usually face-down, for the duration of 2-3 days in order to help the scarring process. The gas bubble will decrease in size over the next few weeks, depending on the gas mixture used during surgery. As long as the bubble is still in the eye, visual acuity is poor and the patient should not undertake any airline flights. If silicone oil was used, it will typically be removed after 3-6 months, but in some cases may be left in the eye permanenty.
A side effect of vitrectomy is the development of a clouding of the lens, called cataract. This usually develops within several months up to few years after surgery. Cataract can be treated effectively with cataract surgery.
What happens during buckle surgery?
This method of surgery used to be the predominant method until 10-20 years ago, but in the meantime has been mostly replaced by the above mentioned vitrectomy. Buckle surgery is typically performed under general anaesthesia. A small silicone sponge is sutured onto the sclera. Sometimes, an encircling band needs to be wrapped around the eye ball. These result in a localized indent of the sclera at the sight of the retinal break to relieve the tension of the viteous gel. Then, a localized freezing (cryopexy) is performed through the sclera to induce scarring at the sight of the break. In some cases, the fluid under the retina needs to be drained through a small opening in the sclera.
What is the prognosis?
The probability of a permanent sealing of the retinal break and an attached retina with the first operation is approximately 85%. With additional surgery, most cases (approximately 97%) can be attached. Prognosis concerning visual acuity after surgery is strongly dependent on whether the centre of the retina (macula) was detached or not. Patients with a complete retinal detachment have a worse prognosis, especially in cases with a long standing detachment and inflammatory signs.
Diabetic Retinopathy
Diabetes is one of the systemic diseases affecting the eyes.
How does diabetes affect the eye?
First not noticable, changes in the blood vessels develop over the course of disease, affecting the eyes as well. Diabetic retinopathy is a chronic micro-vascular disorder of the retina. It affects vision and may lead to blindness.
What is the course of disease?
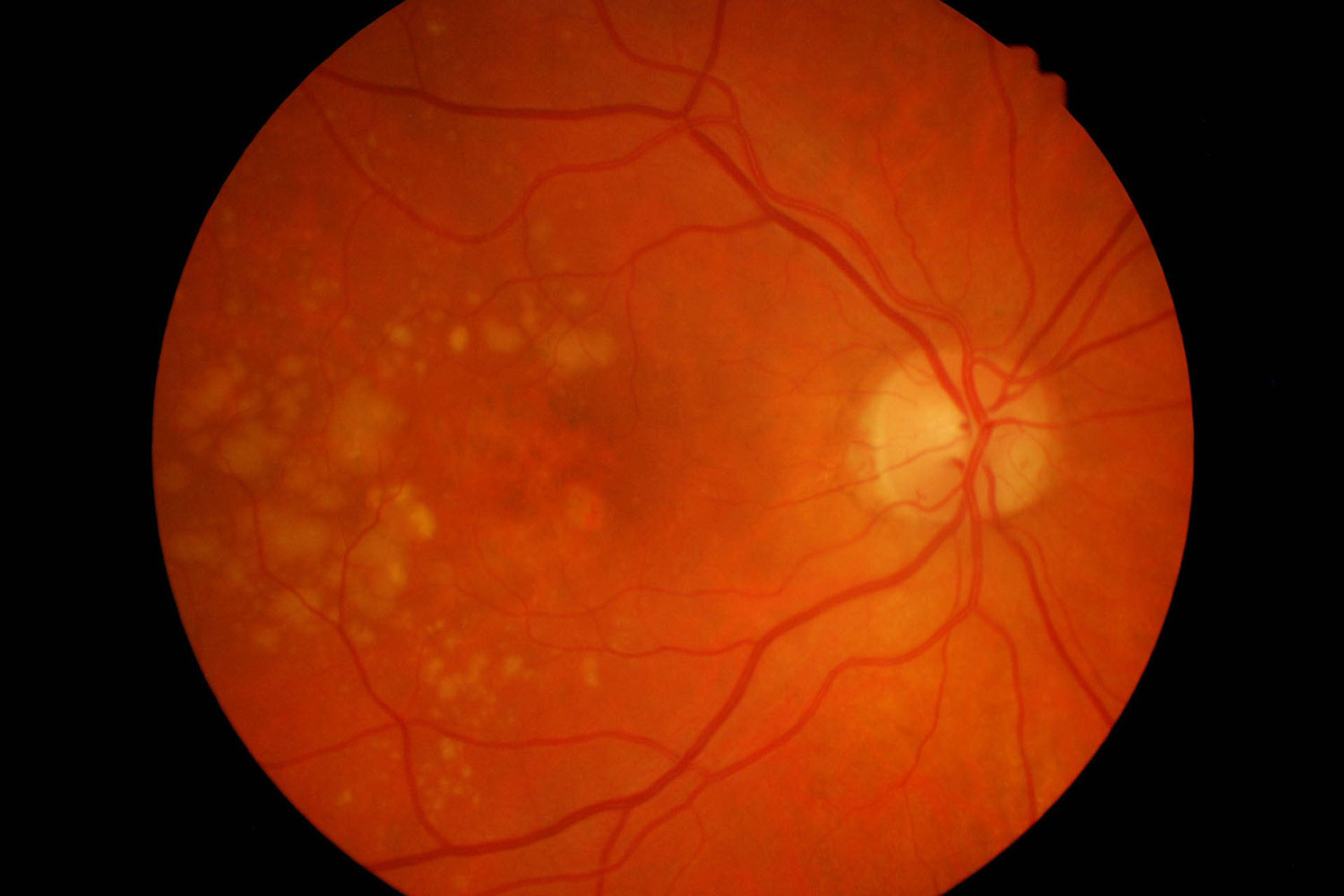
There are two stages of diabetic retinopathy: background retinopathy is the earliest stage in the development of retinopathy. It is characterised by the presence of small haemorrhages, abnormal blood vessels and fatty deposits.
Proliferative retinopathy is the more severe stage of the disease. The smallest vessels, called capillaries, are blocked and starve the retina of nutrients. In response to this, new vessels grow either in front of the retina on to the back surface of the vitreous gel, or occasionally on the iris. The new vessels are fragile and may bleed into the vitreous. This form of retinopathy may eventually lead to blindness.
What are the possible treatments?
So far, diabetic retinopathy cannot be cured, but different forms of treatment may control deterioration. In general, early diagnosed retinopathy followed by an early onset of treatment raises the chances of success.
Early diabetic control may slow down the rate of the progression of complications. If you suffer from diabetes, you can contribute a lot by living a healthy lifestyle. You should control your diet and weight, avoid smoking and alcohol and have your blood sugar levels and your blood pressure checked regularly.
If your ophthalmologist has already diagnosed damage in the retina during the retinal examination, laser treatment may slow down the course of the disease or stop it, reducing the danger of loosing eyesight.
Laser therapy is called photocoagulation. This procedure focuses a laser beam in small bursts onto the damaged retina. The laser treatment reduces the tissue hormones which caused the growth of the new blood vessels. Therefore, the new vessels shrink and this reduces the chance of haemorrhage. Laser treatment is only mildly painful and has to be repeated according to the severitiy of the disease. Treatment is usually performed on an outpatient basis, but in some cases your ophthalmologist may recommend staying overnight.
In some patients where there has been recurrent bleeding and the vitreous is clouded with old or fresh blood, a vitrectomy operation may be necessary. The exchange of the cloudy vitreous with a clear substance can help to restore some vision. Depending on the state of the retina, the quality of your vision may not be as good as it was previously. In some severe cases of diabetic retinopathy, success means stabilising vision and preventing it from getting worse.
Can I prevent diabetic retinopathy?
Early detection and treatment will benefit your eye sight. As there are no noticable symptoms in the early stages of the disease, diabetics should have their eyes checked by an ophthalmologist every year including a complete retinal examination. If diabetic retinopathay is diagnosed, these eye exams have to be repeated in shorter intervals. In most cases, the ophthalmologist will start treatment before the patient experiences visible deteriorations in eye sight.
Diabetic retinopathy is one of the most common causes for blindness in the western world, but it can be prevented in most cases. Please book an appointment at Prof. Findl’s private practice for a thorough examination of your eyes
Filme
Do you have questions about surgery?
Please send an email to office@findl.at including your contact phone number.
Mrs. Findl-Reiffenstuhl will call you back and answer your questions!