The transparent front part of the eye is called the cornea. A variety of corneal diseases may cause clouding of the cornea which may need to be treated using corneal transplantation. During the last decade, surgical techniques for corneal transplantation have improved significantly. Previously, the complete cornea with all its layers was removed and removed with a whole transplant, called PK (penetrating keratoplasty). Nowadays, the new lamellar transplant techniques are the technique of choice when suitable. In these cases, only the layer of the cornea which has the disease, is replaced, whereas the healthy layers are preserved. These lamellar techniques, called DSAEK, DMEK and DALK, have several advantages, such as increased safety during surgery, reduced risk of rejection of the transplant, faster rehabilitation and better visual function after surgery. Prof. Findl performs all modern techniques of DSAEK, DMEK and DALK at Hanusch Hospital.
Eye Surgery
Corneal Transplantation
Corneal Transplantation
Diseases
Diseases of the innermost layer of the cornea: Fuchs’ Endothelial-Dystrophy, Cornea guttata, Bullous Keratopathy
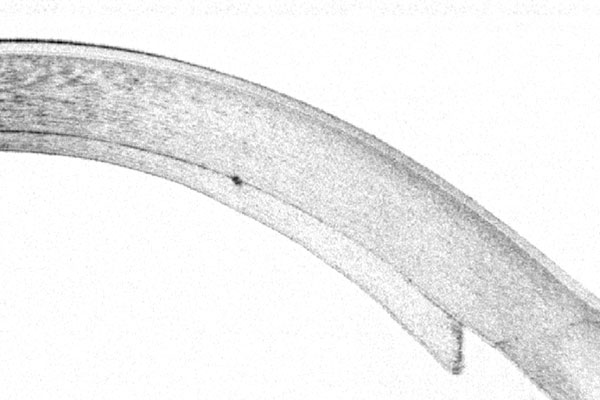
If the innermost layer of the cornea, the endothelial cell layer, is affected, the cornea thickens and becomes cloudy. This disease is called “Cornea Guttata”, and in case of thickening of the cornea, “Fuchs’ Endothelial Dystrophy”. Typically, these diseases appear in the elderly. If endothelial cell loss is caused by previous surgery or trauma, it is called “Bullous Keratopathy”.
What are Ultra-thin DSAEK, DMEK and DWEK surgery?
DSAEK, “Descemet Stripping Automated Endothelial Keratoplasty”, and DMEK, “Descemet Membrane Endothelial Keratoplasty”, are used for diseases of the innermost layer of the cornea. These are Fuchs’ endothelial dystrophy, cornea guttata and bullous keratopathy.
DSAEK, especially ultra-thin DSAEK which Prof. Findl performs, uses a very thin transplant of less than 0.1mm thickness.
DMEK uses only the very thin Descemet membrane introduced as a roll into the eye.
DWEK, „Descemet without endothelial keratoplasty”, (also called DSO, „Descemet Stripping Only“), is used in eyes with cornea guttata and poor vision, but intact endothelial cells in the periphery. With this surgery, the central 4mm zone of Descemet membrane is removed without transplantation of foreign tissue. Only few patients meet the criteria for this type of surgery.
What happens during endothelial transplantation?
This surgery is typically performed in local anesthesia, if only if desired, in general anesthesia. In eyes without previous cataract surgery, the corneal transplantation is usually combined with cataract surgery and lens implantation. Through a small cut of 2-4mm, the innermost layer of the cornea is removed with a special instrument. Then, the donor tissue is cut to the appropriate size and implanted into the eye using special injector systems. The transplant is then pushed against the cornea using an air or gas bubble. The patients need to stay in a supine position (lying flat on their backs) for several hours. The air bubble usually resolves itself within 1-2 days.
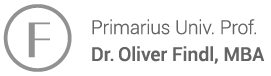
How can a correct position of the transplant be checked?
Prof. Findl uses a high resolution cross sectional image device called OCT, which is integrated into the operating microscope. Prof. Findl was the first to use the prototype of this special microscope worldwide. He can see whether residual fluent is present between the patient’s cornea and the corneal transplant and this reduces the risk of an early transplant detachment.
Diseases of the Corneal Stroma: Corneal Scars, Keratoconus
If the stroma, the main tissue of the cornea, is affected, the surgery of choice is either “DALK” or “PKP”. Corneal scars may be the result of infectious corneal ulcer, herpes keratitis or trauma.
When is DALK used?
If the central layer of the cornea, the stroma, is clouded, which may be the case after severe corneal infections (corneal ulcer, herpes infection), the surgical methods “DALK” (Deep Anterior Lamellar Keratoplasty) and “PK” (Penetrating Keratoplasty) are applied.
DALK and Keratoconus?
In the case of Keratoconus, a disease that typically affects young men and results in corneal thinning of the stroma, “DALK” will be performed if possible. The innermost layer of the cornea stays intact and, therefore, the risk of rejection of the graft is reduced dramatically. The cornea is incised (trephined) partially under general anesthesia. Using a special canula, air is injected into the corneal stroma. This often results in the creation of a “big bubble” that pushes the Descemet membrane backwards. Then the altered corneal stroma can be removed selectively. The healthy Descemet membrane and the endothelial cells stay intact. The donor tissue is then fixated with sutures. The benefit of this new technique is the decreased risk of rejection of the graft in comparison with the conventional corneal transplantation method (PK).
When is PK used?
In cases of severe thinning in progressed Keratoconus as well as eyes with deep corneal scars, the conventional “PK” may still be the surgery of choice. The transplant is also held in place by sutures which are removed in the office (outpatient) typically 1 – 2 years after surgery.
Examination
Corneal Topography
Corneal Topography is used for determining astigmatism with high precision. This device helps to clearly illustrate irregular astigmatism, such as in Keratoconus or after injuries. We also use this examination method when planning cataract surgery in patients with significant astigmatism. In this case, astigmatism has to be measured with precision in order to choose a suitable toric lens.

Films
Corneal Transplantation
You have questions about surgery?
Please send an email to office@findl.at including your contact phone number.
Mrs. Findl-Reiffenstuhl will call you back and answer your questions!